Summary of the PCS Changes and Ambulance Data Collection
The Centers for Medicare and Medicaid Services (CMS) just released a Final Rule outlining changes to the Physician Certification Statement (PCS) requirements and the Ambulance Data Collection System. Both initiatives go into effect on January 1, 2020, so it is critical that ambulance services begin preparing now by updating written and electronic PCS forms and ensuring they are capable of tracking and reporting data that CMS will be requesting over the next four years.
The PCS Changes
Distinction Between Types of Certification Statements
Beginning January 1, 2020, there will be a distinction between a Physician Certification Statement and a Non-Physician Certification Statement. Here’s how it works:
- A Physician Certification Statement is defined as a statement signed by the beneficiary’s attending physician.
- A Non-Physician Certification Statement is defined as a statement signed by an individual other than the beneficiary’s attending physician.
Important Regulatory Note: To accomplish this, CMS added a new paragraph (a) to the regulations at 42 CFR § 410.40 to define a PCS and a non-physician certification statement. So, all of the subsequent paragraphs now change. Most significantly, paragraph (d) “Medical necessity requirements” will be redesignated as paragraph (e) effective January 1, 2020. In addition, CMS is removing all references to a “physician’s order.” The current regulation refers to a “written order from the beneficiary’s attending physician” and states that a “physician’s order must be dated no earlier than 60 days before the date the service.” CMS is removing the references to a physician’s order and beginning January 1, 2020, the regulation will only refer to a “physician certification statement”.
PWW believes that the simplest way to account for these revisions is to change the title of PCS forms by removing the word “Physician” and simply calling the form a “Medical Necessity Certification Statement” or something similar. Whether the form qualifies as a Physician or Non-Physician Certification Statement will simply depend upon who signed the form.
Additional Non-Physician PCS Signers for Transports that are Unscheduled or Scheduled on a Non-Repetitive Basis
Beginning January 1, 2020, the following individuals would also be able to sign for non-repetitive and unscheduled transports:
- Licensed practical nurse (LPN);
- Social workers; and
- Case managers.
As with the other non-physician staff currently permitted to sign non-repetitive, unscheduled PCS forms, LPNs, social workers, and case managers need to be employed by the beneficiary’s attending physician or the hospital or facility where the beneficiary is being treated and from which the beneficiary is transported, and have personal knowledge of the beneficiary’s condition at the time the ambulance transport is ordered or the service is furnished.
Ambulance services who use PCS forms (or an electronic equivalent) will need to update those forms to ensure their form includes these three new signers by January 1, 2020.
Important Note: The new rules does not change the PCS requirements for scheduled, repetitive transports.
Ambulance Data Collection
Effective January 1, 2020 and continuing through 2024, ground ambulance providers and suppliers that have been selected to participate in the Medicare Ground Ambulance Data Collection System must collect and report information on cost, utilization, revenue, and other service characteristics in accordance with the Medicare Ground Ambulance Data Collection Instrument for a continuous 12-month period. The information collected will be used to evaluate the extent to which reported costs relate to payment rates under the Medicare Part B Ambulance Fee Schedule (AFS), as well as to collect information on the utilization of capital equipment and ambulance capacity, and the different types of ground ambulance services furnished in different geographic locations, including rural areas and low population density areas (super rural areas).
Who Will be Selected?
CMS says that ALL ambulance services will eventually be selected and required to submit the survey. CMS is supposed to select a sample each year that is representative of different types of ground ambulance providers and suppliers and different geographic locations. CMS has posted the list of 2664 ambulance services selected to report for Year 1 cost reporting. Ambulance services are selected by NPI, not name, and reporting is based upon unique NPI number. So, if an organization has multiple NPI numbers, it will have to submit a separate report for each NPI when selected.
CMS will sample ground ambulance services that are enrolled in Medicare, and billed for at least one Medicare ambulance transport in the most recent year for which CMS has a full year of claims data prior to sampling. CMS is proposing that 25% of ground ambulance organizations be sampled from all strata (as described below) in each of the first 4 years of reporting. CMS is will stratify the sample based on:
- Provider versus supplier status
- Ownership
- For-profit
- Non-profit
- Government
- Service area population density – transports originating in primarily:
- Urban zip codes
- Rural zip codes
- Super rural zip codes
- Medicare billed transport volume categories of:
- 1 to 200
- 201 to 800
- 801 to 2,500
- 2,501 or more
The Penalty
Beginning January 1, 2022, CMS will apply a 10% payment reduction to a provider or supplier’s Medicare payments if a provider or supplier does not “sufficiently submit” the cost information. The 10% reduction will apply for an entire year that will be specified by CMS and that year is not supposed to be more than 2 years after the end of the period for which the Secretary determines that the ground ambulance provider or supplier failed to sufficiently submit information. CMS is supposed to make a determination that the ground ambulance organization is subject to the 10% payment reduction no later than the date that is 3 months following the date that the ambulance organization’s data reporting period ends. The only exceptions to the 10% penalty is if CMS grants a hardship exemption, or CMS determines through an informal review that the organization is not subject to the 10% reduction to payments.
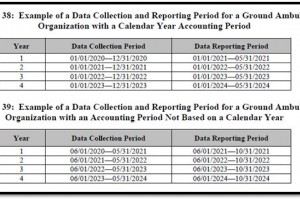
The Data Collection and Reporting Period
Ambulance services will report data over a calendar 12-month period or a “fiscal year” type 12-month period. For the first data collection period, organizations reporting on a calendar year basis will collect data from January 1, 2020 through December 31, 2020, and organizations reporting on a fiscal year basis will collect data over a continuous 12-month period of time from the start of the fiscal year beginning in calendar year 2020. Upon being notified that they are selected as part of the sample, ground ambulance services must notify CMS of their annual accounting period within 30 days according to the instructions in the notification letter. Respondents would also confirm the data collection period when reporting data via the data collection instrument.
Respondents have up to 5 months to report the data to CMS following the end of its 12-month data collection period. For example, if a ground ambulance organization is selected as part of the representative sample for the CY 2020 data collection year, and notifies CMS that its annual accounting period is based on a calendar year, the data reporting period would be January 1, 2021 through May 31, 2021. A ground ambulance organization selected for CY 2020 that notifies CMS that its annual accounting period is based on a fiscal year basis with a fiscal year beginning on June 1, 2020 and ending May 31, 2021 would have a data reporting period from June 1, 2021 through October 1, 2021.
Required Information for Collection and Reporting
Selected ground ambulance organizations must collect and report all information that is applicable to their organization in the Medicare Ground Ambulance Data Collection Instrument. This information will include:
- Organizational Characteristics (NPI, name, type of ownership, category, etc.)
- Service Area (ZIP codes, primary and secondary response areas)
- Emergency Response Time (average response time in primary and secondary area, any response requirements, etc.)
- Ground Ambulance Service Volume (total responses, total transports, paid transports)
- Service Mix (emergency/non-emergency, air, water, ALS/BLS, etc.)
- Labor Costs
- Paid Provider Staff
- Paid Administration, Facilities, Medical Director Staff
- Volunteer Labor
- Facilities Cost
- Facility Information (how many facilities)
- Lease/Mortgage Costs
- Insurance, Maintenance, Utilities and Taxes
- Vehicles Costs
- Ground Ambulance Vehicle Costs
- Non-Ambulance Vehicle Costs
- Other Costs Associated with Vehicles (registration, license, insurance, maintenance)
- Equipment, Consumables, and Supplies
- Medical Equipment/Supplies
- Non-Medical Equipment/Supplies
- Other Costs
- Total Costs and Revenue
- Total costs related to ground ambulance services
- Total revenue from ground ambulance services
- Total ground ambulance service utilization
To more accurately define total costs and total revenues related to ground ambulance services for those ground ambulance organizations that provide other services in addition to ground ambulance services, (e.g., Municipal Fire Departments, Hospital-based providers, etc.) the data collection instrument would further refine costs and revenue into 3 categories to appropriately apportion those costs and revenues. They are:
- Cost and revenue components completely unrelated to ground ambulance services. Examples include administrative staff without ground ambulance responsibilities, health care delivery outside of ground ambulance, community paramedicine, community education and outreach, and fire and police public safety response.
- Cost and revenue components partially related to ground ambulance services. Examples include EMTs who are also firefighters and facilities with both ground ambulance and fire department functions. (They considered an alternative where respondents would allocate costs and report only costs associated with ground ambulance services but believe that would pose an additional burden on the respondent to calculate allocated amounts and would result in an allocation process that is less transparent and standardized).
- Cost and revenue components entirely related to ground ambulance services. Examples include EMTs with only ground ambulance responsibilities and ground ambulance vehicles.
Anticipated Public Availability of Summary Data
Beginning in 2022, and at least once every 2 years thereafter, CMS will post on its website data that it collected under this section, including but not limited to summary statistics and ground ambulance organization characteristics.
MedPAC Report
Not later than March 15, 2023, MedPAC must assess, and submit to Congress a report on, information submitted by providers and suppliers of ground ambulance services through the data collection system, the adequacy of payments for ground ambulance services and geographic variations in the cost of furnishing such services. The report must contain the following:
- An analysis of information submitted through the data collection system;
- An analysis of any burden on ground ambulance providers and suppliers associated with the data collection system;
- A recommendation as to whether information should continue to be submitted through such data collection system or if such system should be revised; and
- Other information determined appropriate by MedPAC.
Learn more about these new rules going into effect January 1 at our December 5 webinar!
